Introduction
Dental implant surgery is typically a staged process designed to replace missing teeth with stable, natural‑looking restorations. Here’s what reputable sources say about preparation, the procedure, and recovery—so you know what to expect before your consultation.
This is general information, not medical advice. Individual timelines and steps vary. Always follow your surgeon’s instructions.
Before Your Procedure
Your clinician will examine your mouth, review your medical history and medications, and take imaging (often 3D) to understand bone, nerve, and sinus anatomy. You will discuss whether placement will be immediate or staged, if bone grafting or a sinus lift is needed, and what type of restoration will be used. The anesthesia or sedation plan and infection‑prevention protocols will also be reviewed so you know what to expect on the day of surgery.
Day of Surgery: Common Steps
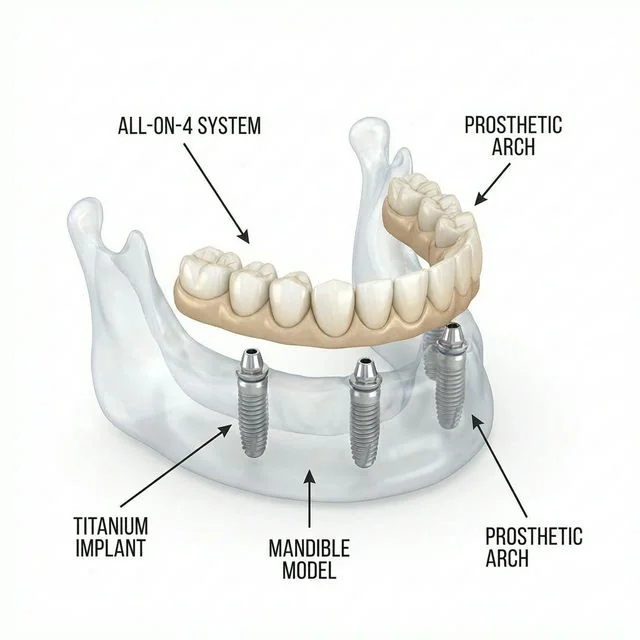
On the day of surgery, anesthesia or sedation is provided as planned. The implant site is prepared and the implant is placed into the jawbone; when needed, grafting or a sinus procedure may be completed at the same time. A healing abutment or cover screw is placed, and you’ll leave with clear instructions for hygiene, diet, and medications during early recovery.
Healing and Osseointegration
After placement, bone integrates with the implant over a healing period. Your clinician will decide when it is appropriate to connect the abutment and take steps toward the final crown, bridge, or full‑arch prosthesis. Scheduled follow‑ups allow the team to monitor healing and adjust the timeline as needed.
After the Procedure: What You Might Experience
It’s common to notice temporary swelling, minor bleeding, and discomfort that improves over the first few days. If grafting or a sinus procedure was part of treatment, you may receive additional precautions to protect healing. Reach out to your clinician promptly if symptoms worsen or do not follow the expected course.
Long‑Term Care and Maintenance
Excellent daily hygiene and regular professional cleanings are essential to reduce the risk of peri‑implant disease. Factors like plaque control, smoking, a history of gum disease, residual cement, and prosthetic design can influence risk. Your clinician will tailor maintenance recommendations to your situation.
Typical Timeline (Varies by Case)
Most treatments move through four stages: evaluation and planning, implant placement, a period of healing for osseointegration, and finally abutment connection with delivery of the crown, bridge, or full‑arch prosthesis. Your dentist will explain how these steps apply to your case and the expected timeline.
Risks and Potential Complications
As with any procedure, there are risks, including infection, bleeding, or involvement of nearby anatomical structures depending on the site. Over time, biological or mechanical issues such as peri‑implant disease or component wear can occur. Individual health, habits, and adherence to maintenance influence these risks.
Self‑Care After Surgery
Follow your clinician’s specific guidance on diet, hygiene, and medications. Keep the area clean as directed and avoid smoking to support healing. Attending scheduled follow‑ups helps ensure recovery is on track and allows timely adjustments to your care plan.
When to Contact Your Dentist
Get in touch if pain or swelling increases after the initial recovery period, if you develop fever or persistent bleeding, or if any components feel loose or uncomfortable.